People that have an immune system that is TH1 dominant are more likely to develop conditions like:
- Multiple Sclerosis
- Hashimoto’s Thyroiditis
- Grave’s Disease
- Crohn’s Disease
- Psoriasis
- Rheumatoid Arthritis
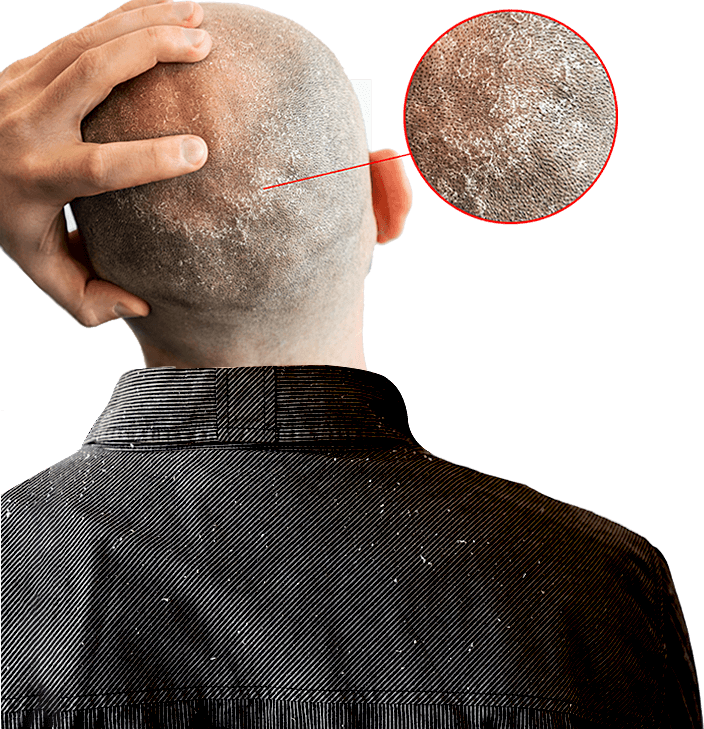
Seborrheic dermatitis is a chronic skin condition that mainly affects the scalp and face. More specifically, it tends to affect parts of the body that have a high number of oil glands. This includes the T-Zone of your face, such as the forehead, eyebrows, the region between the eyebrows and the nose (nasolabial folds). Seborrheic dermatitis also has the tendency to affect the scalp, ears, eyelids, chest and upper back.
The symptoms tend to come and go with varying periods of flareups and remission. Once you develop seborrheic dermatitis, not only can it last for decades, it can also significantly affect your health and your daily life.
Seborrheic dermatitis is often incorrectly portrayed as a condition that is similar to dandruff, eczema, psoriasis and other types of dermatitis. It is important to know that the treatments which work for these other conditions rarely work for seborrheic dermatitis. That’s because seborrheic dermatitis is a unique condition with its unique set of causes and its own unique treatment.
Here are some signs that can help you easily recognize your seborrheic dermatitis…
There are two main things that define seborrheic dermatitis:
Which looks like dandruff or thick plaques. These plaques can be stuck to your skin or be peeling off.
That causes skin redness and pain. The redness usually occurs in patches instead of being uniform all over.
We can find the answer to this by taking a closer look into how our skin is composed and how it functions.
So, let’s dive even deeper and take a closer look at the epidermis because that will tell us what goes wrong with our skin during seborrheic dermatitis…
Note that as more and more new skin cells are born at the bottom of the epidermis, the older cells are pushed up through the different layers until they get to the very top and die. These dead skin cells are then slowly shed off the skin surface to make way for new dead skin cells.
This journey that the skin cell takes, from being born at the bottom of the epidermis to dying and being shed at the very top, takes about 27 days. This process is called cellular turnover.
Now what do you think would happen if something shortened this journey from 27 days to say 13-15 days? You would get dandruff.
You see, the new skin cells that were constantly being made would be getting pushed up to the surface way too fast. Once at the surface, these skin cells would not be ready to be shed. This would cause those skin cells to start piling up at the very top. This skin cell pileup is what we call dandruff.
But what if we went one step further and made things even worse?
What if we shortened the journey the skin cells take up to the surface
from 27 days and shortened it even more to about 9-10 days? you would now have seborrheic dermatitis.
The skin cell pileup at the very top would be so bad that it would look like thick plaques. And that’s exactly what happens during seborrheic dermatitis – the cornified layer at the very top of the epidermis becomes thicker and hyperkeratinized (too much keratin builds up there).
Furthermore, if you looked closely inside the skin of a seborrheic dermatitis sufferer, you would see another interesting thing.The epidermis would be infiltrated with immune system cells causing inflammation as if your skin was under some threat. This is what causes the redness and irritation during seborrheic dermatitis flareups.
If you kept track of how your skin behaved over the course of a few months, you would notice that there would be periods of normal behavior where the skin cells travel at a normal pace to the surface to be slowly shed and there would be no sign of inflammation-causing immune system cells infiltrating the epidermis. Then you would suddenly notice the skin behaving abnormally with the cellular turnover getting shorter and the immune system cells infiltrating the epidermis, causing inflammation
In other words, there would be some sort of a switch turning the condition on and off at random times, forcing you to go from remission to flareups over and over again.
So, this begs the question…
What is it that turns this switch on and off at random times in your skin ?
It turns out, there’s not one but 5 different things that activate this switch.
Yes, there are 5 different causes of seborrheic dermatitis and it is critical to know what they are because successfully overcoming your condition comes down to treating each one of these 5 causes effectively.
For decades we have been given a disease model for seborrheic dermatitis that was both incomplete and inaccurate. Even worse, almost all commonly available treatments today are based on this outdated understanding of the problem.
However, thanks to continued research, we have discovered that there are 5 things at the root of seborrheic dermatitis and the only way to find long-term relief is to treat all 5 of these root causes at the same time.
Let’s take a look at what the most current research says are the 5 main causes of seborrheic dermatitis:
Seborrheic dermatitis was first clinically described in 1887 and seven years later the same researcher found that behind this skin condition was a yeast called Malassezia. Ever since then, Malassezia has been blamed as the main cause of seborrheic dermatitis.
Indeed, Malassezia is found in higher quantities in the areas of the skin where you have active seborrheic dermatitis flareups. We’ve even figured out how this yeast triggers a flareup in seborrheic dermatitis sufferers:
![]()
![]()
![]()
![]()
![]()
![]()
![]()
This leads to a vicious cycle where the free fatty acids further increase the growth of Malassezia, which in-turn further increases the skin’s permeability, which allows more of the irritant metabolites to get deeper into the skin, which further increases the inflammation and worsens your skin scaling.
It seems clear that Malassezia is undeniably behind seborrheic dermatitis. In fact, that’s the theory we’ve worked with and based our treatments on for over a century.
However, there’s just one problem…
If this were all that was causing your seborrheic dermatitis, you simply would need to get rid of the yeast and the oils on your skin and the problem would be resolved. As a matter of fact, that’s how we’ve been treating the problem all along
But as we know, this strategy rarely provides long-term relief and for some reason the flareups keep getting worse with time for most sufferers.
Certainly, something else is at play. Something we aren’t fixing.
It just so happens that there are indeed other things behind seborrheic dermatitis – other causes we didn’t know of before and have only recently discovered…
Recent studies have shown that seborrheic dermatitis is as much an immune system disorder as it is a skin condition. In fact, if you looked closely at your skin during a flareup, you’ll notice that it looks like your skin is having an allergic reaction to something.
Indeed, one of the main causes behind seborrheic dermatitis is an immune system imbalance.
Let’s see what this imbalance is…
Imagine our immune system having two parts that act like two sides of a seesaw. One side (TH1) is responsible for eliminating harmful pathogens like viruses and bacteria that get inside our cells and the other side (TH2) helps protect us against harmful things like allergens and toxins that that invade the space outside our cells.
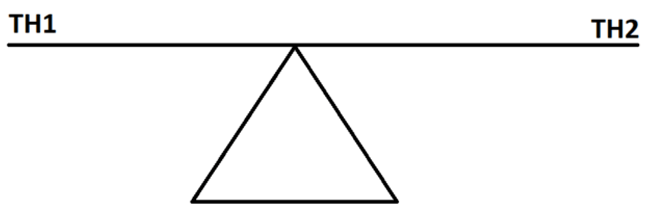
When one side becomes dominant and goes up, the other side tends to weaken and go down. To maintain a healthy body you need to make sure that both the TH1 side and TH2 side balance each other out.
But what if something causes the balance to tip to one side? You would be more likely to develop certain types of diseases.
People that have an immune system that is TH1 dominant are more likely to develop conditions like:
People that have an immune system that is TH1 dominant are more likely to develop conditions like:
That’s why seborrheic dermatitis flareups behave like your body is having an allergic response and that’s exactly what is happening inside your skin.Histamine levels tend to be chronically elevated in dandruff sufferers. These higher levels of histamine increase the production of IL-17 and TH17 which traps the sufferer in a cycle of worsening inflammation, deeper allergen invasion into the skin and a more aggressive allergic response.
And what is this allergen that constantly triggers an allergy-like response in seborrheic dermatitis sufferers?
The Malassezia yeast and the byproducts it makes when it feeds on your skin oils
Just imagine your immune system constantly trying to eliminate a yeast that quickly repopulates your skin no matter how many times you try to clear it with antifungals? It’s like leaving the allergy switch on all the time.
And how do we know any of this is true?
How do we know that it really is an over-sensitive immune system that is constantly reacting to the otherwise harmless Malassezia?
Because during clinical studies when we decreased the TH2 side of the immune system in seborrheic dermatitis sufferers using probiotics, they suddenly became “less allergic” to Malassezia and showed a significant reduction in their symptoms.
Have you ever noticed that when you are in the middle of a seborrheic dermatitis flareup, only certain regions of your skin experience the scaling and irritation. If Malassezia is present all over our scalp and face, why does the irritation and scaling only occur in specific patches while the neighboring parts between these patches are left unaffected? Shouldn’t our entire scalp and face be evenly affected all over?
It just so happens that these affected patches where your skin is flaking and irritated are also the regions where the Malassezia yeasts clump together. The reason why these yeasts overwhelmingly clump together in these specific regions is because the skin cells here have a defect.
Studies have shown that the skin cells of seborrheic dermatitis sufferers have a compromised defense mechanism; which limits their ability to keep harmful substances from entering the deeper layers of your skin. It is believed that these skin cells might have filaggrin deficiency that impacts the skin barrier.
Think of the defective skin cells as weak doorways in your otherwise fortified skin wall made up of tough corneocyte (dead skin cell) bricks. Interestingly, the yeast on your skin are able to somehow detect where these weak doorways are present and begin to gather there.
Now, these gathered yeast may not always be able to make it through and you may find some rest (remission). But sooner or later, these weak doorways fail and the yeast come rushing in, penetrating the skin and triggering an immune system attack (flareup).
And so, you have repeated episodes of remissions and flareups with the skin constantly refortifying itself and the yeast repeatedly clumping around defective skin cells and making their way in.
It almost looks like we have put all the puzzle pieces together and have a good scientific explanation for why seborrheic dermatitis happens.
But there’s just one more lingering problem…
Our skin doesn’t just rely on one barrier to defend itself from harmful substances. There are in-fact multiple barriers that work together to neutralize microbial threats like Malassezia.
So why don’t these other barriers protect us against Malassezia? The answer to this brings us to the 4th cause of seborrheic dermatitis…
Since our skin is constantly exposed to all sorts of threats in our environment, our body has devoted many resources to defend it. This is why our skin is protected by not one but four key barriers:
These 4 barriers are critical for protecting us from almost every type of threat in the outside world.
During seborrheic dermatitis all 4 of these barriers fail.
Let’s see how…
Failure of the physical barrier – The topmost layer of our skin (stratum corneum) is composed of flattened dead skin cells called corneocytes. These toughened corneocytes come together to form a strong physical barrier that protects us from physical, biological and chemical threats.
However, as we saw earlier, there corneocytes of seborrheic dermatitis sufferers have a defect which weakens their ability to shield our skin from harmful substances. The Malassezia yeast takes advantage of this defect and breach the physical barrier, making their way deeper into the skin and triggering an immune system attack (flareup).
Failure of the flora barrier – Just the way our gut has bacteria that live inside it and play an active role in its normal function, our skin too has both bacteria and fungi that dwell on the surface and constantly interact with it. And just like our gut, the good bacteria and fungi on our skin help keep the bad bacteria and fungi in-check by outcompeting them for space and nutrients.
But during seborrheic dermatitis, not only does the Malassezia yeast on our skin begin to overgrow, it turns against us (pathogenic). This disrupts the protective microbiome (bacteria) and mycobiome (fungi) of our skin and leads to a failure of the flora barrier.
Failure of the moisture barrier – If you think of the dead skin cells on our skin surface as bricks, then the mortar between these bricks is something called the extracellular lipid membrane. Think of this lipid membrane like a fatty glue that not only holds the dead skin cells together, it also forms a water-proof barrier. This barrier keeps our skin moist by preventing the loss of water (and electrolytes), it prevents infections and the lipids also regulate the shedding of the dead skin cells off the top of our skin.
When you are in the middle of a seborrheic dermatitis flareup, the Malassezia yeast feeds on your skin oils and produces free fatty acids (FFA). These free fatty acids penetrate the top layer of your epidermis and disrupt the extracellular lipid membrane. This leads to trans-epidermal water loss and causes your protective moisture barrier to fail.
Failure of the pH barrier – Our skin maintains a very thin acidic film on the surface that protects us from viruses, bacteria, fungi and toxins. This thin film, also known as the acid mantle, plays a vital role in the normal functioning of our skin, including the synthesis and aggregation of lipids, how the skin cells mature and are shed from the epidermis, the composition of our skin’s microbiome (bacteria) and mycobiome (fungi) and the activation of many protective proteins
While the pH of this acidic barrier should ideally be between 5.8 to 4.1, research indicates that people with seborrheic dermatitis tend to have higher a skin pH (more alkaline). This higher skin pH weakens the integrity of the stratum corneum (top layer of the epidermis), it also affects corneocyte cohesion causing the dead skin cells to dissociate more easily from each other. Finally, the higher skin pH stimulates something called the proteinase-2-activated receptor which ends up causing the skin to be chronically irritated.
With the loss of all 4 of these critical barriers, your skin is left extremely vulnerable. Now add to this the fact that our skin always harbors a microbe (Malassezia) that constantly looks for opportunities to take advantage of this vulnerability and it becomes clear why seborrheic dermatitis is so difficult to overcome
We’ve long known that people with gut issues also tend to have skin problems. For example, IBD patients are much more likely to develop psoriasis and people with H. Pylori infections in their stomach are more susceptible to rosacea. However, it has only recently come to light that there may be a gut dysfunction behind seborrheic dermatitis as well.
Emerging data has revealed that our gut influences our skin health via something known as the gut-skin axis. In fact, research shows that there are two particular issues of the digestive tract that can make someone prone to seborrheic dermatitis:
Gut Dysbiosis – Which is an imbalance of gut bacteria that leads to poor gut health. and
Intestinal Barrier Dysfunction – Where your gut essentially becomes “leaky” and loses its ability to keep harmful toxins and microbes out
Let’s take a closer look at both these issues…
Gut Dysbiosis – According to new research, our gut bacteria play a major role in the functioning of our skin by affecting three things:
All three of these things are central to seborrheic dermatitis
Evidence suggests that seborrheic dermatitis sufferers have altered skin microbiomes and this may be the result of an altered gut microbiome (dysbiosis). We know this because when we improve the gut microbiomes of seborrheic dermatitis patients by feeding them healthy bacteria, it reinforces their skin barrier function, it decreases their skin sensitivity and it modulates their skin’s immune system, returning their skin back to normal.
Intestinal Barrier Dysfunction – There are many parallels between our skin and our gut…
For example…
And just the way disruptions in our gut’s microbiome disrupts our skin’s microbiome, disruptions in our gut’s barrier function also disrupts our skin’s barrier function. One way this can happen is when the gut’s barrier becomes compromised, it allows harmful bacteria and its metabolites to enter our blood stream and accumulate in the skin. Among these harmful metabolites are phenols and bioactive toxins that impair the maturing of young skin cells by reducing a key protein called Keratin 10. This causes our skin’s protective moisture barrier to lose its integrity, making us vulnerable to seborrheic dermatitis.
Furthermore, people with an intestinal barrier dysfunction also show abnormal levels of a protein called defensin which has also been associated with the development of seborrheic dermatitis.
As you can see, emerging research has completely transformed our view of why seborrheic dermatitis happens and what is the best way to treat it. However, what’s even more surprising are new findings about how seborrheic dermatitis can harm us.
So next, let’s take a look at the long-term dangers of seborrheic dermatitis that have only recently come to light.